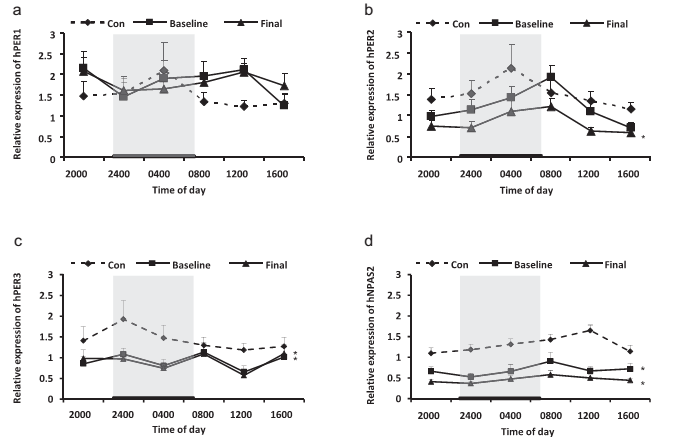
Plasma peptide and hormone levels in healthy controls and schizophrenia patients. (a) Cortisol. (b) Orexin. (c) Insulin. COR, cortisol; OX, orexin; INS, insulin. The data are expressed as mean ± SEM. n = 13 for schizophrenia patients. n = 15 for healthy controls. *p < 0.05, different from controls; #p < 0.05, different from baseline. Con: controls. Baseline, before clozapine treatment; Final, after 8-week clozapine treatment.
精神分裂症患者存在着诸如睡眠-觉醒、激素和神经肽分泌的近日节律紊乱,近日节律由节律基因调控。然而精神分裂症患者节律基因表达的近日节律是否有异常目前尚不清楚。抗精神病药氯氮平治疗前后精神分裂症患者节律基因表达和激素、神经肽分泌的近日节律的变化尚不明确。
陆林课题组收集了来自15个健康男性对照和13名男性精神分裂症患者血液样本,精神分裂症在治疗前和治疗第8周末分别在24小时内每隔4小时采集一次5ml外周静脉血。健康对照只进行一个24小时的外周静脉血标本采集。采用Real-time PCR测定hPER1、hPER2、hPER3、hNPAS2基因mRNA的表达量和放射免疫法测定Cortisol、Insulin、Orexin血浆浓度。结果发现与正常对照组相比,精神分裂症患者出现PER1,PER3和NPAS2等节律基因的表达和食欲素的释放失调。伴随PER2表达出现延迟,PER3和NPAS2的表达减少,皮质醇水平增加。这些节律基因失调(例如,在PER1和PER3表达)在氯氮平治疗8周时仍持续存在。氯氮平治疗8周可显著降低24小时hPER2 mRNA表达水平,增加24小时血浆胰岛素的水平。结果说明,8个星期的氯氮平治疗后出现持续的神经生物学变化可能有助于预测精神分裂症长期维持治疗的复发率和治疗效果。
Hong-Qiang Sun, Su-Xia Li, Fang-Bin Chen, Yan Zhang, Peng Li, Mei Jin,Yan Sun, Fan Wang, Wei-Feng Mi, Le Shi, Jing-li Yue, Fu-De Yang, Lin Lu*(2015). Diurnal neurobiological alterations after exposure to clozapine in first-episode schizophrenia patients. Psychoneuroendocrinology .